What should we eat—and not eat—to lower the cardiovascular disease risk factor lipoprotein(a)?
Lipoprotein A, also known as Lp(a), is an independent, genetic, and causal factor for cardiovascular disease and heart attacks. At any level of LDL cholesterol, our risk of heart attack and stroke is two- to three-fold higher when our Lp(a) is elevated. With a high enough Lp(a) level, atherosclerosis continues to progress even if we get our LDL cholesterol way down, which may help explain why so many people continue to have heart attacks and strokes even under treatment for high cholesterol. It’s been suggested that “it would be worthwhile to check Lp(a) levels in a patient who has suffered an event but has no traditional risk factors to explain it.” What’s the point of checking it, though, if there isn’t much we can do about it? “To date, no drug to reduce circulating Lp(a) levels has been approved for clinical use.”
Some researchers blame our lack of knowledge on the fact that Lp(a) is not found in typical lab animals, like rats and mice. It’s only found in two places in nature: primates and hedgehogs. Hedgehogs? How strange is that? No wonder Lp(a) is “an enigmatic protein that has mystified medical scientists ever since” it was first discovered more than half a century ago. But who needs mice when you have men? The level in our bloodstream is “primarily determined” by genetics. For the longest time, Lp(a) was not thought to be significantly influenced by factors such as diet. Given its similarity to LDL, though, one might assume lifestyle changes, “such as increased physical activity or the adoption of a healthy diet,” would help. “However, the effects of these interventions on Lp(a) concentrations are so far either only marginal or lacking in evidence,” but might that be because they have not tried a plant-based diet yet?
As I discuss in my video How to Lower Lp(a) with Diet, when it comes to raising LDL cholesterol, we’ve known for years that the trans fats found in meat and dairy are just as bad as the industrially produced trans fats found in partially hydrogenated oil and junk food. But, when it comes to Lp(a), as you can see below and at 2:05 in my video, trans fats from meat and dairy appear to be even worse.
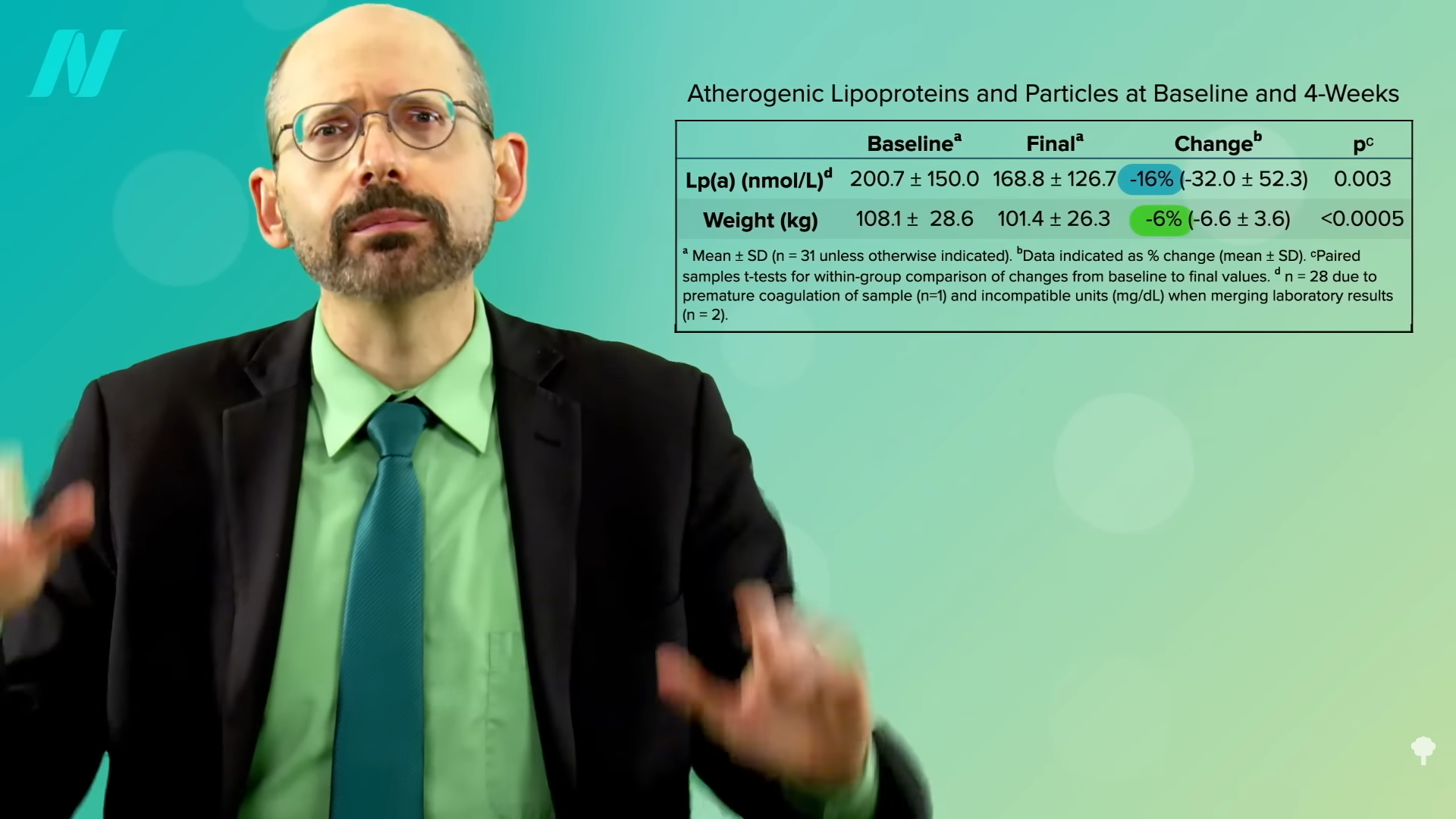
Just cutting out meat and following a lacto-ovo vegetarian diet did not appear to help, but, as you can see below and at 2:19 in my video, when study participants were put on a whole food, plant-based diet packed with a dozen servings of fruits and vegetables a day, their Lp(a) levels dropped by 16 percent within four weeks.
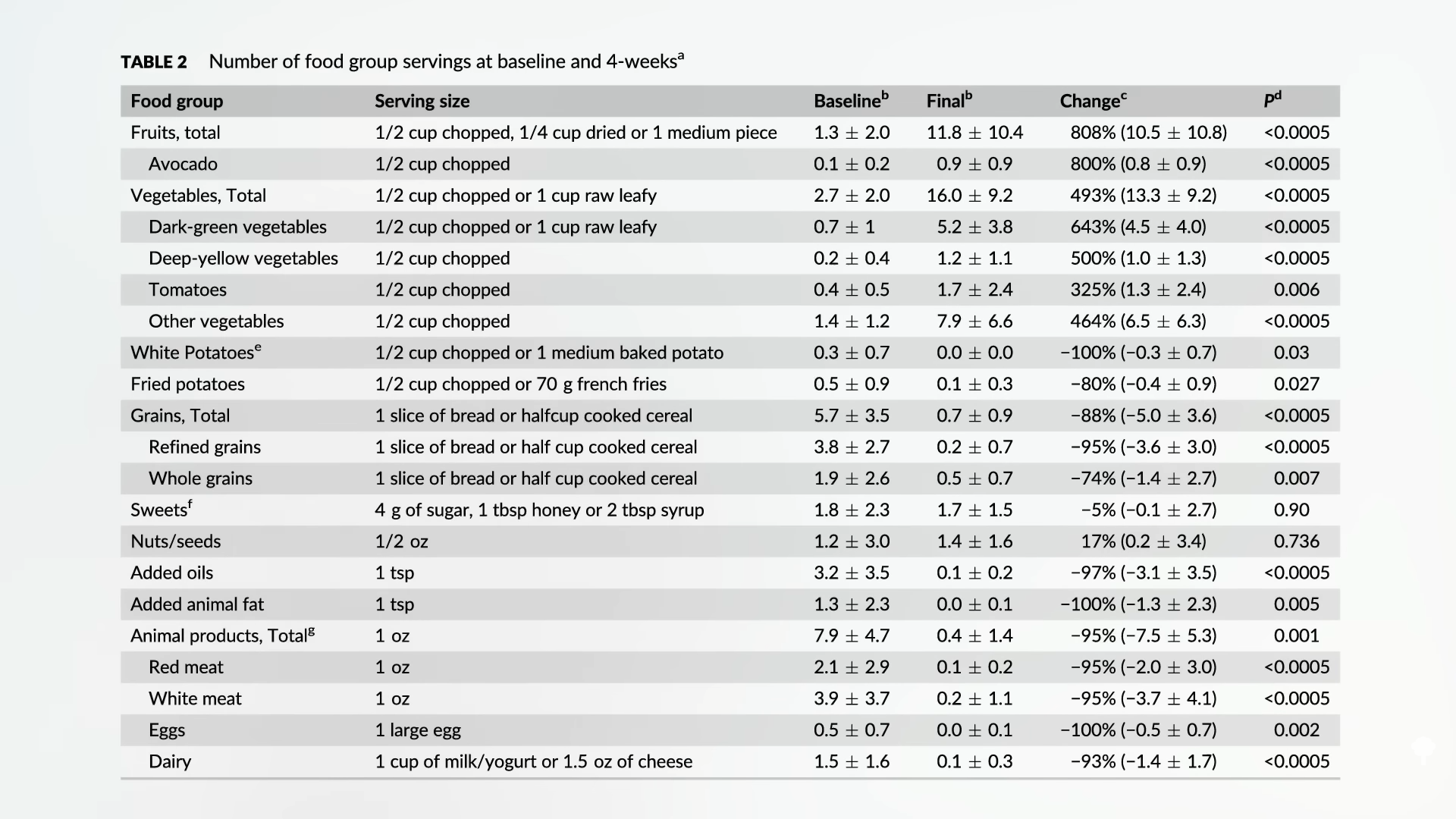
Of course, in those 30 days, the study subjects also lost about 15 pounds, as you can see below and at 2:28, but weight loss does not appear to affect Lp(a) levels, so you figure that it must have been due to the diet.
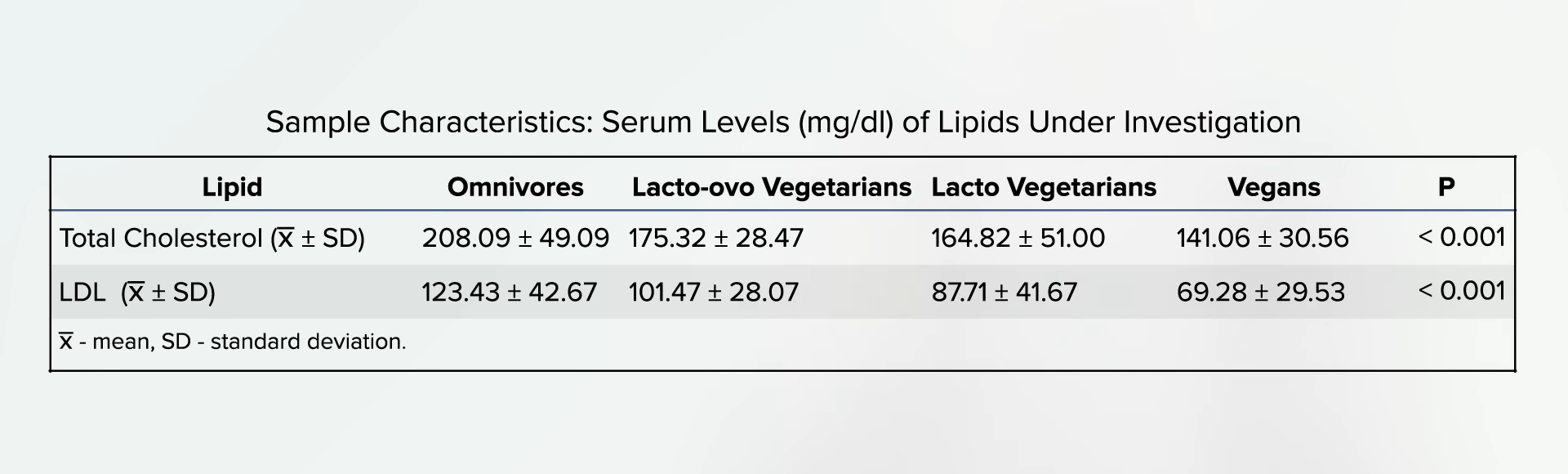
If you’re already eating a healthy plant-based diet and your Lp(a) levels are still too high, are there any particular foods that can help? As with cholesterol, even if the average total cholesterol of those eating strictly plant-based may be right on target at less than 150, with an LDL under 70, there’s a bell curve with plus or minus 30 points that fall on either side, as you can see below and at 2:45 in my video.
Enter the “Portfolio Diet,” which is not only plant-based, but also adds specific cholesterol-lowing foods—so, think nuts, beans, oatmeal, and berries to drag cholesterol down even further. The infographic is below and at 3:11 in my video.

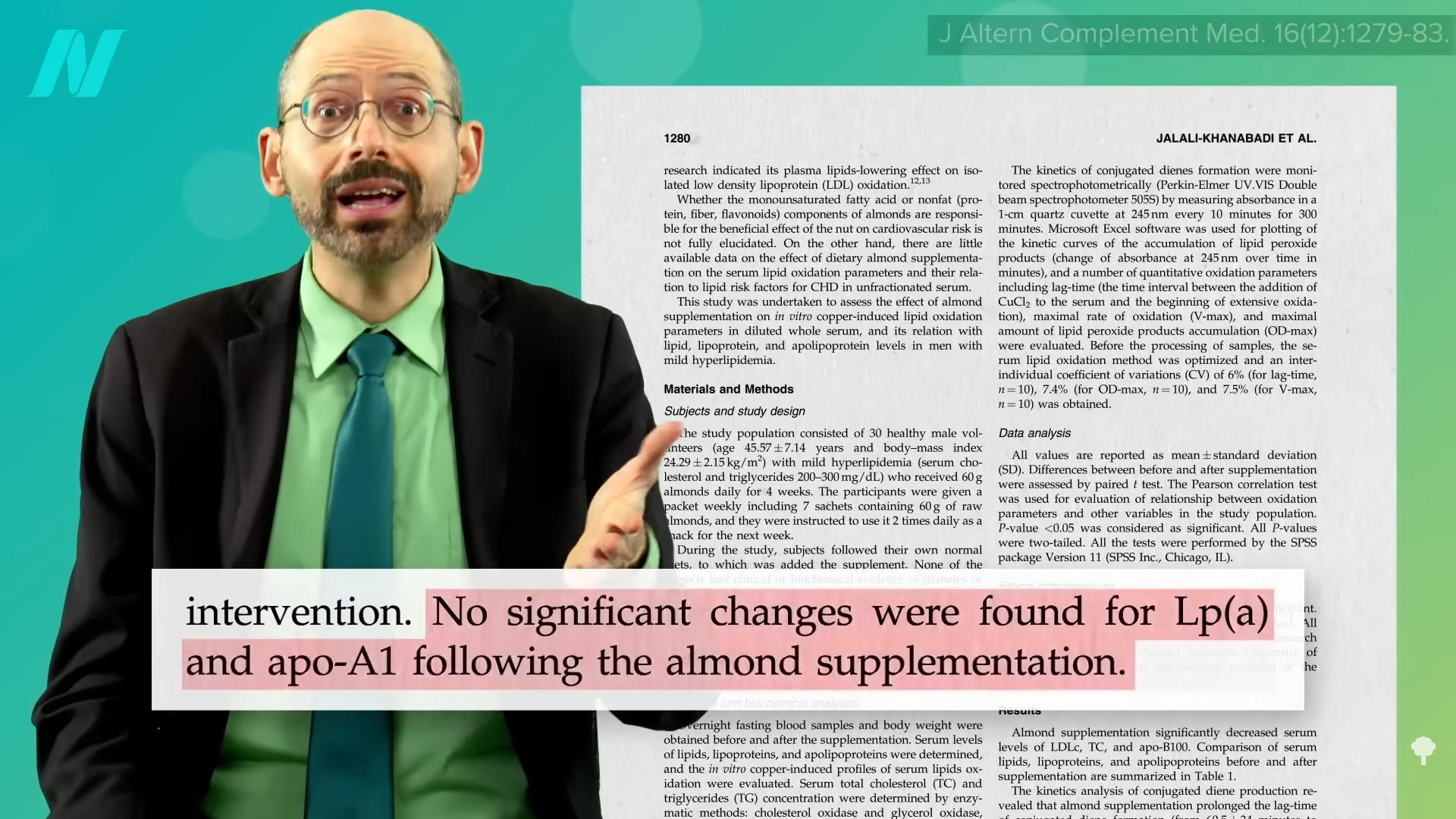
What about Lp(a)? Nuts have been put to the test. Two and a half ounces of almonds every day dropped levels, but only by about 8 percent. That is better than another nut study, though, that found no effect at all, as you can see below and at 3:29 in my video. An additional study found “no significant changes,” and researchers reported that subjects in their study “did not experience a change in Lp(a).” Ah, nuts.
There is one plant that appears to drop Lp(a) levels by 20 percent, which is enough to take people exceeding the U.S. cut-off down to a more optimum level. And that plant is a fruit: Emblica officinalis, otherwise known as amla or Indian gooseberry. A randomized, double-blind, placebo-controlled study asked smokers before and after the trial about their “mouth hygiene, cough with expectoration, shortness of breath on exertion, loss of appetite, feelings of impending doom, palpitation, sleep deprivation, irritability, heartburn and tiredness,” as well as such objective measurements as their blood count, cholesterol, DNA damage, antioxidant status, and lung function. The amla extract used “showed a significant improvement compared to the placebo group in all the subjective and objective parameters tested with no reports of adverse events.” No side effects at all. That’s unbelievable! No, that’s unbelievable. And indeed, it’s completely not true.
Yes, subjective complaints got better in the amla group, but they got better in the placebo group, too, with arbitrary scoring systems and no statistical analysis whatsoever. And, of the two dozen objective measures, only half could be said to reach any kind of before-and-after statistical significance and only three were significant enough to account for the fact that if you measure two dozen things, a few might pop up as positive if only by chance. Any time you see this kind of spin in the abstract, which is sometimes the only part of a study people read, you should suspect some kind of conflict of interest. However, no conflicts of interest were declared by the researchers, but that’s bullsh*t, as the study was funded by the very company selling those amla supplements! Sigh.
Anyway, one of those three significant findings was the Lp(a), so it might be worth a try in the context of a plant-based diet, which, in addition to helping with weight loss, can dramatically improve blood pressure (even after cutting down on blood pressure medications) and contribute to a 25-point drop in LDL cholesterol. Also, it may contribute to a 30 percent drop in C-reactive protein and significant reductions in other inflammatory markers for “a systemic, cardio-protective effect”—all thanks to this single dietary approach.
You may be interested in my video on Trans Fat in Meat and Dairy. Did you know that animal products are exempted from the ban? See Banning Trans Fat in Processed Foods but Not Animal Fat.
For more on amla and what else it can do, check out the related posts below.
If you missed my previous video on Lp(a), watch Treating High Lp(a)—A Risk Factor for Atherosclerosis.

